
Robotic assisted laparoscopic prostatectomy is a
minimally invasive surgery to remove the prostate
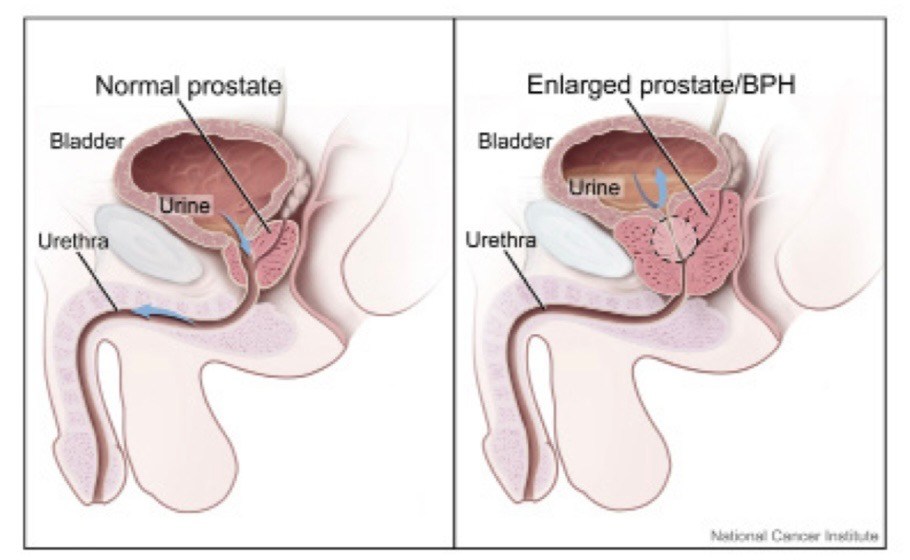
New York, N.Y. — Robotic Prostate Surgery has two types—the radical version is for prostate cancer, and the simple version is for benign prostatic hypertrophy, a condition in which the prostate gland is enlarged but not cancerous.
Mount Sinai doctors performed the first robotic radical prostatectomy in New York. This operation uses a state-of-the-art robotics surgical system to remove the prostate through a few small incisions instead of one large incision, as was traditionally done in the open surgical approach.
At Mount Sinai, where they use their Precision Urology approach, they focus on integration of multiple variables and imaging data in a decision support system. This is key in assuring men with prostate cancer of our commitment to a patient-centric, personalized diagnostic approach and excellent outcome while minimizing the side effects of treatment.
Precision Urology reflects Mount Sinai’s utilization of advanced technologies and incorporation of molecular and genomic analysis to identify markers of aggressive disease. This allows them to rigorously stage disease to determine if intervention is needed and if so, tailor the treatment accordingly.
Robotic Prostate Surgery Technique: ART
The robotic prostate surgery approach used by Dr. Tewari is known as ARTT (Advanced Robotic Technique) prostatectomy.
This is a highly successful approach to curing prostate cancer while minimizing side effects in select patients. Dr. Tewari and his team have developed and refined ART over the past decade based on the thousands of surgeries they have performed, their discoveries in prostate anatomy, and other leading-edge research.
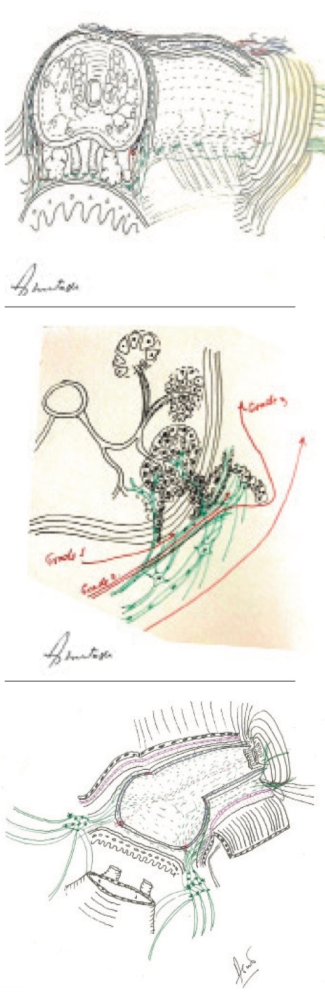
ART is highly individualized, reflecting a patient’s unique anatomy, cancer location and neural structure. Indeed, for Dr. Tewari, ART is truly an art. He routinely makes anatomical drawings of prostates on which he operates in order to map out a cancer’s spatial relationships to the fascia, muscles and nerves that surround the prostate.
By drawing the anatomy of individual cases, he continues to fine tune ART™ and improve cancer control while sparing nerves. He also uses the drawings as a teaching tool for students as well as his peers worldwide who are eager to learn his technique.
The crux of the ART technique is the delicate removal of the prostate from the top of the nerve hammock with maximal clearance for preserving sexual and urinary function. Not only are nerves not handled, but oxygenation of the nerves is monitored during this phase of the technique so these preserved nerves are greater in number and also healthy and vascular.
The ART approach consists of not just one technique but a group of techniques, including those for diagnosis. Mount Sinai uses a new state-of-the-art technique known as targeted biopsy, to precisely diagnose prostate cancer. This technique fuses highly detailed MRI (magnetic resonance imaging) with real-time ultrasound using the Artemis device.
The procedure typically takes 15 to 20 minutes and is done in Mount Sinai offices under local anesthesia. It provides highly accurate information about the location of cancer and its relation to nerves and sphincters. Mount Sinai is one of a few medical facilities in New York City with the Artemis device.
Outcomes
Cancer control – ART™ has proven to provide low margin rates (less residual cancer). As a consequence, there is less need for radiation and hormone therapy post surgery and men have less reason to feel anxious about future rises in their PSA.
Benefits
Robotic prostate surgery is extremely precise, which offers a variety of benefits over traditional (open) prostate surgery, including:
. • Smaller incisions
• Shorter hospital stay
• Less pain
• Less risk of infection
• Less blood loss and transfusions
• Less scarring
• Faster recovery
• Superior cancer control
• Superior nerve sparing
In addition, with robotic prostate surgery, a temporary catheter remains in place for considerably less time (five to seven days instead of two weeks), and there is less risk of urinary incontinence and impotence following the robotic prostate surgery procedure.
This approach results in complete removal of cancer for nearly 95% of all patients whose cancer is confined to the prostate.
In published long-term follow-up studies performed by Mount Sinai Urology Chair Ashutosh (“Ash”) K. Tewari, MD, this also means that these patients have an extremely good chance (95%) of reaching the 10-year survival mark.
Robotic prostate cancer surgery is extremely safe in experienced hands, but some complications are possible in any abdominal procedure. Possible complications may include bleeding, infection, blood clotting, heart attack, hernias, permanent urinary incontinence, impotence, and strictures.
While intraoperative mortality is almost unheard off, it is possible with any anesthesia and surgery. Equipment malfunction is rare, happening in less than 0.4% of cases; Mount Sinai has three backup robots to address this remote possibility.
Surgical Outcomes
Mt. Sinai reports that they usually evaluate the outcome of primary prostate cancer treatment by looking at cancer control, preservation of urinary continence, and preservation of sexual function. The Advanced Robotic Technique, developed by Dr. Tewari, is highly successful on all three measures, producing minimal disruption to your daily life.
. • Cancer control is the ability of the surgeon to remove all cancerous tissue from the body. Mt. Sinai measure this by looking at the surgical margins (the rim or border of the tissue removed in surgery). Once they complete the procedure, they send the prostate to the Pathology Department to test for margins and cancer grade (of any remaining malignancy). If the margins are “clean” or cancer-free, they assume that we have removed all of the malignant tissue and we have achieved cancer control.
• Urinary incontinence is determined by whether the bladder and surrounding anatomy are unaffected by removal of the prostate.
• Sexual potency is about sexual functioning, a chief concern of men undergoing prostate cancer treatment.
da Vinci Robot
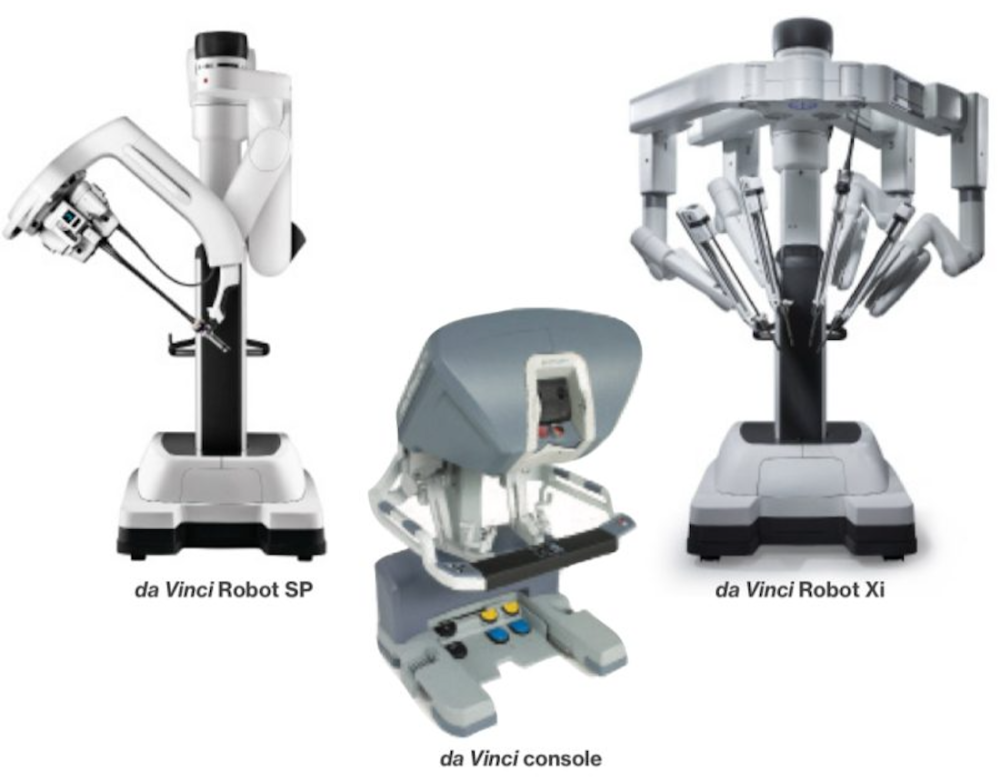
The da Vinci surgical system is a sophisticated robotic platform designed to expand the surgeon’s capabilities and offer a state-of-the-art minimally invasive option for prostate surgery.
With da Vinci, small incisions are used to insert miniaturized instruments and a high-definition 3-D camera. Seated comfortably at the da Vinci console, Dr. Tewari views a magnified, high-resolution 3-D image of the surgical site inside the body.
At the same time, the latest robotic and computer technologies scale, filter, and seamlessly translate Dr. Tewari’s hand movements into precise micro-movements of the da Vinci instruments.
Although it is often called a “robot,” the da Vinci surgical system cannot move or operate on its own; Dr. Tewari is 100 percent in control.
Faster return to urinary continence
ART incorporates a novel surgical technique to minimize or prevent urinary leakage, even with exertion, and provide a strong urinary stream. It involves reconstruction of the supporting structures responsible for urinary continence that are typically either removed or disorganized during removal of the prostate.
Dr. Tewari developed a detrusor wrap procedure that creates an additional wrap that serves as a sphincter and sling to provide enhanced and accelerated return to continence. Most of our patients who are continent before the surgery are continent 18 months after surgery.
Hood technique
Dr. Tewari performs approximately 400 robot-assisted radical prostatectomies every year.
The procedure takes around 30-40 minutes, with an additional 30 minutes for real-time pathology. When removing the prostate, we want to leave as much of the prostate’s surrounding tissue intact as possible, as this will minimize the disruption of urinary mechanisms.
The surgical technique used at Mount Sinai allows for careful separation of the detrusor apron from the anterior prostate. The detrusor apron allows the bladder to store urine, and contracts during urination to release urine. It overlies the prostate and extends from the bladder neck to the pelvis. Because the detrusor apron covers this important area, we call this area, and the procedure we do to protect it, the “Hood.”
In addition, with the ART technique, patients and their families have been able to benefit from faster convalescence, shorter hospital stays, small incisions with less scarring, significantly less blood loss during surgery, and less pain following surgery. The majority of our patients are discharged and return home within 24 hours of their robotic surgery.
Outcomes and Implications
Less than 10% of men experience complications after prostatectomy, and these are usually treatable or short-term. The two most common post-surgery problems are urinary incontinence and erectile dysfunction. Less than 5% of men younger than age 50, and less than 15 percent of men age 70 or older, are incontinent after radical prostatectomy.
Most men are able to have sex after prostatectomy while using ED medicines (such as Viagra or Cialis), an external pump, or injectable medications. The younger the man, the higher the chance of maintaining potency after prostatectomy. A period of penile rehabilitation is often necessary.
Sparing the nerves that can cause urinary incontinence or erectile dysfunction is the hallmark of a skilled surgeon. A patient who has a radical prostatectomy by a surgeon at an advanced prostate cancer center has a better chance of maintaining sexual and urinary function.
Cancer control – ART has proven to provide low margin rates (less residual cancer). As a consequence, there is less need for radiation and hormone therapy post surgery and men have less reason to feel anxious about future rises in their PSA.
High rates of erectile function recovery – The aim of ART is to preserve every nerve fiber responsible for the fine balance between erection, orgasm, and bladder function.
The benefits of the ART technique for sexual function are significant. ART™ allows for stronger erections and orgasms, a reduction in penile shrinkage and a reduction in the risk of climacturia (involuntary release of urine at the moment of orgasm).
In order to protect the delicate nerves involved, which do not handle heat, traction, or manipulation very well, Mount Sinai usse a nerve-sparing, completely athermal and “traction free” technique (no use of cautery or heat energy) during robotic prostatectomy- a technique pioneered by Dr. Tewari and his team. A majority of their patients who experience normal sexual functioning and are candidates for nerve-sparing, return to normal sexual function after ART surgical treatment.
The best case scenario at Mount Sinai is when patients are young, cancer is early and organ-confined, and baseline sexual functions are very high. Dr. Tewari can perform Grade I nerve-sparing that can achieve excellent potency (ability to have intercourse) with or without use of oral medications.